As major countries in the world are struggling to contain COVID-19 pandemic, the approach taken by South Korea to flatten the infection curve through extensive testing has received significant attention. The country was able to manage the rising incidence of COVID-19 without going into a complete lockdown since the government adopted a Real-time Reverse transcriptase-polymerase chain reaction (rRT-PCR) as the method of choice and effectively implemented large-scale testing. Steps were taken for fast authorization and improved access to these tests, setting up drive-through testing facilities, and effective management of patients who tested positive.
Currently, as governments in many countries are trying to follow the model, a country’s ability to conduct extensive testing has been accepted as a critical factor to successfully contain the outbreak. Tests based on RT-PCR are considered as the gold standard at present and the world is struggling to improve access to these tests.
Why RT-PCR?
Viruses adopt multiple means to dampen host defense. Symptoms of the infection can be confusing as viral mechanisms to evade host immune system responses often overlap. For instance, COVID-19 starts with generic symptoms such as slight cough, mild fever, etc., posing a significant challenge to differentiate it from various other respiratory diseases including the common cold.
SARS-CoV-2, the virus causing COVID-19, is a betacoronavirus. It uses the Angiotensin-converting enzyme 2 (ACE2) receptor, which is present in almost all human organs, as the main entry path to infect humans. The infection can be mild or asymptomatic in many patients even though they may carry similar viral loads like that of symptomatic patients, making disease containment highly challenging. Hence, diagnostic methods need to have high specificity to differentiate SARS-CoV-2 from other similar viruses.
At present, a large number of tests being rolled out for COVID-19 diagnosis are based on RT-PCR, since the method can offer high sensitivity and specificity for an accurate diagnosis. The full sequence of SARS-CoV-2, an RNA virus, became available since early January 2020 enabling the development of RT-PCR tests by various groups worldwide.
Designing RT-PCR Assays for COVID-19 Diagnosis
SARS-CoV-2 has about 30,000 nucleotides, which encodes 27 proteins. The proteins that are being considered for diagnosis include RNA-dependent RNA polymerase (RdRP) in the open reading frame ORF1ab region and four structural proteins. The RdRP is a highly conserved gene among coronaviruses. The structural proteins of SARS-CoV-2 include the spike surface glycoprotein (S), small envelope protein (E), matrix protein (M), and nucleocapsid protein (N).
[box title=”” border_width=”2″ border_color=”#81d742″ border_style=”solid” align=”center” ]
“S genes have better sensitivity to pick up COVID-19 in nasopharyngeal swabs“
[/box]
The S protein enables the virus to infect cells by mediating its attachment to the host cell surface receptors. The S gene of SARS-CoV-2 has <75% nucleotide similarity with other SARS-related coronaviruses. A recent study published in The Lancet on January 24, 2020, indicates that S genes have better sensitivity to pick up COVID-19 in nasopharyngeal swabs.
The E protein is an integral membrane protein, which also plays a major role in many stages of the life cycle of the virus. Similarly, while N protein is vital for making up the nucleocapsid, it is also involved in handling other aspects including the virus replication cycle and the host cellular response to viral infection. M protein defines the shape of the viral envelope and is also involved in organizing the viral assembly with other structural proteins. Compared to the S gene, the other three structural proteins are more conserved among coronaviruses.
According to the World Health Organisation (WHO) guidelines published in March 2020 routine confirmation of COVID-19 cases needs to be based on the detection of unique sequences of SARS-CoV-2 RNA using nucleic acid amplification (NAAT) tests such as RT-PCR. The tests need to contain at least two different regions on the SARS-CoV-2 genome, of which at least one is preferably specific for the virus. RdRP, N, E, and S genes are highlighted as the viral genes commonly targeted for diagnosis. Multiplex assays are preferred with at least two gene targets, where one is a universal primer for coronaviruses, while the second primer is specific for SARS-CoV-2.
RT-PCR Tests in the Market for COVID-19
The initial protocols published by WHO include the one by Charité Institute of Virology in Germany for detecting E gene for screening and RdRP as well as N genes for confirmation. Many more rRT-PCR assays have entered the market through emergency use authorization (EUA) route.
GenoAmp RT-PCR Assays for COVID-19 Diagnosis
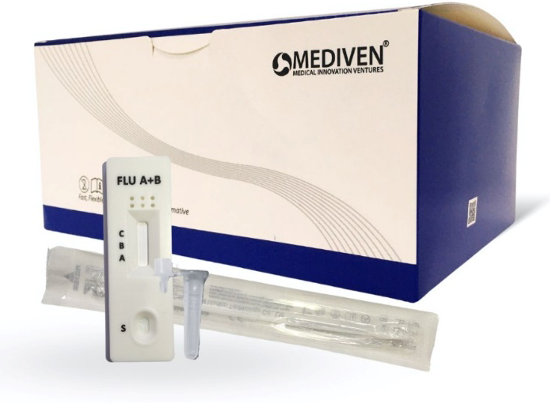
Medical Innovation Ventures Sdn Bhd (Mediven) has been at the forefront of the fight against SARS-CoV-2 in Malaysia. The company offers GenoAmp® Real-Time RT PCR Flu A/Flu B/SARS-CoV-2/MERS-CoV kit for screening and differentiation of human influenza A and B strains, SARS-CoV-2 and MERS-CoV from clinical samples. Another COVID-19 diagnostic product offered by Mediven is GenoAmp® Real-Time RT-PCR SARS-CoV-2 kit, which utilizes RdRP and S genes for screening and N gene for confirmation. The spike gene offers the test better sensitivity in diagnosing SARS-CoV-2 in nasopharyngeal swabs.
[box title=”” border_width=”2″ border_color=”#81d742″ border_style=”solid” align=”center” ]
“Mediven’s multiplex RT-PCR assay targets RdRP, S and N genes for fast and accurate COVID-19 diagnosis”
[/box]
Both the assays are in line with WHO guidelines and enable accurate and fast diagnosis of COVID-19. The Malaysian government expedited the evaluation process of Mediven’s COVID-19 diagnostic kits for meeting the rising demand for accurate and extensive testing in the country.